
We developed URApp to aid adherence to bladder training in young people (aged 10-19 years) with urinary incontinence and urgency. Urinary incontinence (UI) is among the most common paediatric problems and it is commonly assumed to resolve with age. Consequently, parents and clinicians often adopt a ‘wait and see’ approach to childhood UI1. A significant proportion of children, however, continue to suffer from persistent UI into adolescence2-5.
The perceived stigma of UI in adolescence can seriously undermine a young person’s self-esteem and quality of life. Some young people with UI suffer from depressive symptoms, bullying, and problems at school6, 7.
“Always thinking about it, always worrying about it”
“…kind of feeling like an outsider, I suppose, feeling that you’re not normal”
“It’s the sheer fact that I have to lie constantly and I’m hiding. I feel like it’s a huge secret”
Young people who are being treated for UI often report poor treatment experiences including a lack of continuity in care, high rates of relapse, and treatment failure. This can lead to feelings of hopelessness8.
“When I’m at the hospital it’s always a new person and they always say a different thing to what the other doctor said”.
“For quite a lot of the time, I felt really pessimistic about this problem, just like there is absolutely no hope that it’s ever going to be better and I’m going to be stuck with this problem forever”.
The majority of cases of UI in young people are not due to organic (structural, anatomical or neurological) causes but arise from functional impairments in the bladder9. Bladder training (standard urotherapy) is the first-line treatment for UI in children and adolescents10. It is a behaviour modification intervention that aims to establish a regular schedule of drinking and toilet visits.
The goal is to ‘train’ the bladder to hold more urine and to reduce the number of times patients need to pass urine per day. Bladder training also educates patients about how the bladder works and common causes of UI, as well as providing guidance on how to have good posture whilst emptying the bladder (e.g. sitting up straight and relaxing the pelvic floor).
There is evidence that bladder training can be an effective intervention for UI in children and adolescents11, 12. However, it takes time to be effective and success strongly depends on adherence, self-motivation and clinician support, which our research shows is often lacking8.
Our research with young people with UI found that adherence to bladder training is often challenging. Clinicians recognise that young people need ongoing support tailored to their needs to enable them to effectively manage their bladder symptoms.
“Urotherapy, which is the mainstay of treatment, requires considerable effort, motivation and self-discipline, which may be difficult for adolescents”
“As a clinician who has worked for years in the incontinence field, it’s clear to me that adolescents require more bespoke understanding, management and care”
In response to this need, we developed a smartphone app (URApp) to aid adherence to bladder training in young people with UI.
We co-designed URApp with extensive input from young people and a team including expert clinicians, health psychologists, health technology design experts, and app developers. Co-designing URApp with young people will help to ensure it is age appropriate, acceptable and usable.
In developing URApp, we were guided by the Person-Based Approach to planning, optimising, evaluating and implementing behavioural health interventions13. This approach involved participatory co-design workshops and in-depth interviews with young people with continence problems to understand and accommodate their needs. We also worked closely with clinicians to ensure that URApp performs the functions needed to support bladder training.
We identified user requirements for URApp at three participatory co-design workshops with young people with UI (see below for examples).
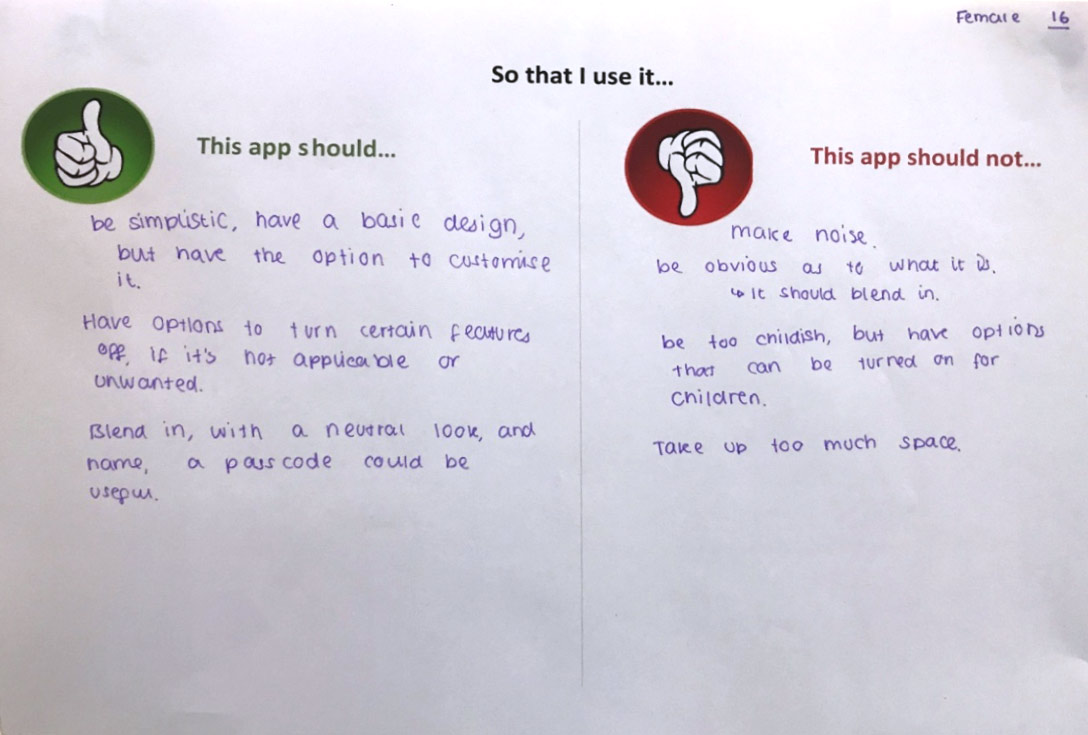
The goals of the workshops were to define the desired behaviour changes (e.g. regular drinking and toilet visits) and to identify factors that influence these behaviours (e.g. restricted access to toilets and drinks during class). The figure below shows some of the designs proposed by young people.
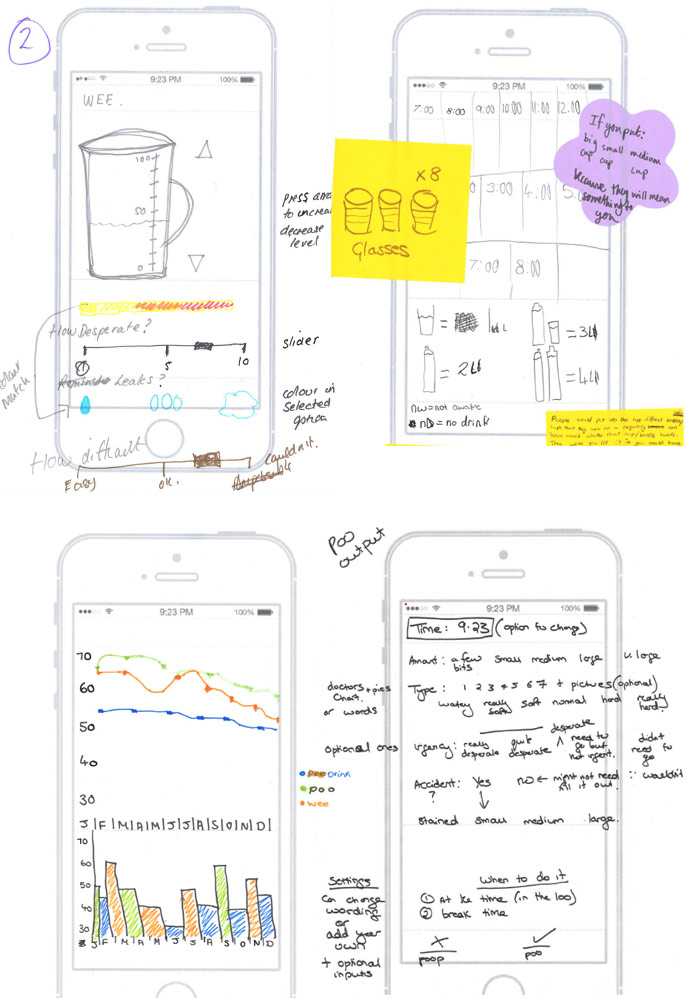
We also identified behaviour change techniques – strategies aimed at changing behaviours (e.g. goal setting and reviewing, action planning, reminders, rewards) to include in URApp that could promote adherence to bladder training (see figure below). There is evidence that embedding behaviour change techniques into digital interventions increases their effectiveness14.

URApp allows users to set goals for their daily drinking and provides discreet reminders to help them to establish a regular schedule of drinking and toilet visits. There is also a diary function to record daily drinking and toilet visits, and personalised feedback to enable users to track progress towards their drinking goals. URApp provides ‘rewards’ (stars and trophies) to motivate users to keep using the app and to achieve their drinking goals.
We investigated the usability and acceptability of URApp through in-depth qualitative research with young people.
“Much better than paper diaries…I never got around to filling them out, whereas this would be on my phone, which I would have on me, so I think that’s a lot handier”
“It makes you feel more committed to achieving your goals… You achieve stuff… It makes you feel good about yourself”
“The most motivating things for me were seeing my progress over time and charting the data”
Young people who have tried URApp found that it helped them to manage their daytime wetting.
“It got a lot better. During the day I stopped having accidents. My symptoms were getting better each week”
“I drink more in the mornings now, rather than lots before bed if I haven’t had enough, which can be problematic at night-time”
“It helped me drink more regularly and space my drinks out throughout the day”
We also interviewed clinicians who treat young people with UI to gain an in-depth understanding of their views of URApp to ensure that they will have confidence in it and will want to use it in clinical practice.
“I think we would use it on every single child that came to our clinic, anyone that came to bladder training, we would direct them all to it and say this is part of it”
“I’m already thinking of kids I could use this with”
We are currently planning to evaluate URApp in paediatric continence clinics to test its effective in improving adherence to bladder training.
References
- Berry AK. Helping children with nocturnal enuresis: the wait-and-see approach may not be in anyone’s best interests. Am J Nurs 2006;106:56–63.
- Heron J, Grzeda MT, von Gontard A, Wright A, Joinson C. Trajectories of urinary incontinence in childhood and bladder and bowel symptoms in adolescence: prospective cohort study. BMJ Open. 2017;7(3):e014238.
- Yeung CK, Sreedhar B, Sihoe JD, et al. Differences in characteristics of nighttime enuresis between children and adolescents: a critical appraisal from a large epidemiological study. BJU Int 2006;97:1069–73.
- Swithinbank LV, Brookes ST, Shepherd AM, et al. The natural history of urinary symptoms during adolescence. Br J Urol 1998;81(Suppl 3):90–3.
- Hellström AL, Hanson E, Hansson S, et al. Micturition habits and incontinence at age 17—reinvestigation of a cohort studied at age 7. Br J Urol 1995;76:231–4.
- Whale K, Cramer H, Joinson C. Left behind and left out: The impact of the school environment on young people with continence problems. Br J Health Psychol. 2018;23(2):253-277.
- Grzeda MT, Heron J, von Gontard A, Joinson C. Effects of urinary incontinence on psychosocial outcomes in adolescence. Eur Child Adolesc Psychiatry. 2017;26(6):649-658.
- Whale K, Cramer H, Wright A, Sanders C, Joinson C. ‘What does that mean?’: a qualitative exploration of the primary and secondary clinical care experiences of young people with continence problems in the UK. BMJ Open. 2017;7(10):e015544.
- Hjälmas K. Functional daytime incontinence: definitions and epidemiology. Scand J Urol Nephrol Suppl 1992; 141: 39–46.
- Chang SJ, Van Laecke E, Bauer SB, von Gontard A, Bagli D, Bower WF, Renson C, Kawauchi A, Yang SS. Treatment of daytime urinary incontinence: A standardization document from the International Children’s Continence Society. Neurourol Urodyn. 2017;36(1):43-50.
- Schäfer SK, Niemczyk J, von Gontard A, et al. Standard urotherapy as first-line intervention for daytime incontinence: a meta-analysis. Eur Child Adolesc Psychiatry. 2018;27(8):949-964.
- Assis GM, Silva CPCD, Martins G. Urotherapy in the treatment of children and adolescents with bladder and bowel dysfunction: a systematic review. J Pediatr (Rio J). 2019;95(6):628-641.
- Yardley L, Morrison L, Bradbury K, Muller I. The person-based approach to intervention development: application to digital health-related behavior change interventions. J Med Internet Res. 2015 Jan 30;17(1):e30.
- Web T, Joseph J, Yardley L, Michie, S. Using the Internet to Promote Health Behavior Change: A Systematic Review and Meta-analysis of the Impact of Theoretical Basis, Use of Behavior Change Techniques, and Mode of Delivery on Efficacy. J Med Internet Res. 2010; 12(1): e4.
